Trauma, Mental Health, & Compassion Fatigue
Trauma
Facts about Trauma and Substance Use
- More than half of substance-using women pregnany women have a PTSD diagnoses compared to 11% of the general population.
- 55-99% of women in treatment for SUD report past trauma exposure (SAMSHA)
- Over 50% of pregnant women with SUD have PTSD symptoms
Symptoms of Post-Traumatic Stress Disorder (PTSD)
To be diagnosed with PTSD, an adult must have all of the following for at least 1 month:
- At least one re-experiencing symptom
- Flashbacks—reliving the trauma over and over, including physical symptoms like a racing heart or sweating
- Bad dreams
- Frightening thoughts
- At least one avoidance symptom
- Staying away from places, events, or objects that are reminders of the experience
- Avoiding thoughts or feelings related to the traumatic event
- At least two arousal and reactivity symptoms
- Being easily startled
- Feeling tense or “on edge”
- Having difficulty sleeping, and/or having angry outbursts
- At least two cognition and mood symptoms
- Trouble remembering key features of the traumatic event
- Negative thoughts about oneself or the world
- Distorted feelings like guilt or blame
- Loss of interest in enjoyable activities
Trauma Informed Care
How can providers help women manage trauma?
- Provide a supportive, safe space to talk about trauma
-
Educate caregivers about Trauma and PTSD
-
Encourage self-soothing and other positive activities: relaxation, meditation, exercise, yoga, prayer, quiet music, spend time in nature
-
Encourage self-compassion
-
Help caregivers learn to interrupt trauma reactions
-
Encourage caregivers to develop other safe spaces and trust people to talk with
-
Interact with sensitivity
-
Learn what you can do to help Moms feel safe
-
Be consistent and trustworthy – Show mom’s that you are following through on discussed plans and that you are a reliable support
-
Seek to understand WHY they are doing or avoiding something
-
Be collaborative, strengths-focused and empowering
-
Trauma Resources
- SAMHSA – Trauma and Violence: https://www.samhsa.gov/trauma-violence
- SAMHSA's Concept of Trauma and Guidance for a Trauma-Informed Approach: https://store.samhsa.gov/product/SAMHSA-s-Concept-of-Trauma-and-Guidance-for-a-Trauma-Informed-Approach/SMA14-4884.html
- Trauma screening tools - https://www.integration.samhsa.gov/clinical-practice/screening-tools#TRAUMA
- Tulane University Traumatology Institute- https://tulanetraumatologyinstitute.com/
Mental Health
Common Comorbidities with Substance Use
- About 50% of people who experience a mental illness, also experience a Substance Use Disorder (SUD) at some point in their life
- About 29% of women with SUDs have co-occurring mood disorders, and 26% have co-occurring anxiety disorders.
- Women with eating disorders often have comorbid SUD (~ 40%)
- Common risk factors can contribute to both mental illness and substance use disorders.
- Some genes convey risk for both SUDs and mental illness
- Environmental factors such as trauma and stress can also contribute to both SUDs and mental illness.
- Some mental health conditions have been identified as risk factors for developing a substance use disorder; people will often use substances to self-medicate
How Mental Health and Trauma Comorbidities affect Mom and Baby Relationships
- Avoidance - Mothers with comorbid issues are more likely to avoid issues related to bonding and parenting
- Misinterpretation - Moms will often misinterpret cues from their babies. For example, when a baby is suffering from residual symptoms of neonatal abstinence syndrome (NAS), and is thus easily startled and crying often, a Mom may interpret this as "My baby doesn't like me."
- Low motivation - a history of trauma and past negative experiences can lead caregivers to feel worn down and may lead to low motivation.
- Hopelessness - feeling hopeless is a symptom of many mental illnesses including depression and is common in this population.
- Irritability - Irritability is also a symptom of many mental illnesses as well as withdrawal from most substances and can interfere with parenting abilities.
For more information on mental health, visit our mental health curriculum page.
Emergency Hotlines
National Suicide Prevention Hotline: 1-800-784-2433 or 1-800-273-8255
Grassroots 24-hour crisis hotline: (410)-531-6677 or 1-800-422-0009
Sources
1. Greenfield, S. F., Back, S. E., Lawson, K., & Brady, K. T. (2010). Substance abuse in women. Psychiatric Clinics, 33(2), 339-355.
2. Comorbidity: Substance Use Disorders and Other Mental Illnesses, NIDA retreived from: https://www.drugabuse.gov/publications/drugfacts/comorbidity-substance-use-disorders-other-mental-illnesses
Compassion Fatigue
Definitions
Compassion Fatigue: Emotional residue from working with those suffering from the consequences of traumatic events. It is the slow loss of ability to empathize with other people and is a general loss of physical and emotional energy. See more symptoms below. It can co-exist with burnout.
Burnout: An unintentional endpoint due to chronic stress in the work environment. Burnout can include symptoms of the following:
- Emotional Exhaustion: Emotional resources depleted by intense needs of clients, workplace, supervisor
- Reduction in sense of accomplishment: Feelings of inadequacy when clients don’t respond to efforts to help
- Depersonalization: Emotional detachment from clients and coworkers
Compassion fatigue and burnout can occur from exposure to one case or many cases. Compassion fatigue is also known as “vicarious” or “secondary” traumatization. It can look like PTSD (intrusive thoughts, nightmares, irritability, avoidance, hypervigilance)
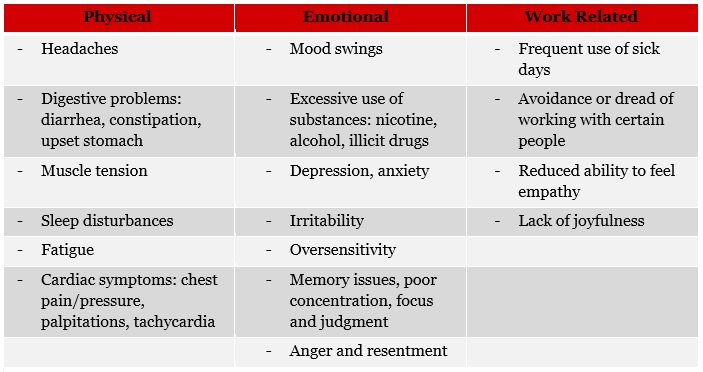
Signs and Symptoms of Compassion Fatigue
Different phases of Compassion Fatigue
Zealot Phase
- Initial phase of enthusiasm when you feel you are making a difference in your profession. You may work late, put in extra hours, or go the extra mile with tasks and demands.
- Though you may be over stressed, you make excuses and justify the stress by reflecting on your professional experience.
- You may recognize that you are beginning to lose control, so you push through by working harder thinking the fulfillment will ease your stress and make the bad feelings disappear.
- When the stress starts to catch up with you, you may experience difficulty breathing, increased heart rate, aches and pains, dizziness, shock, and sweating.
Irritability Phase
- In the irritability phase, you may begin noticing behaviors at work such as daydreaming and becoming distracted, an increase in mistakes and oversights, and cutting corners.
- You may notice changes in your personality such as a loss in your sense of humor. You may be more cynical and critical of others, resorting to mocking them and criticizing them unfairly.
- Overall in this phase, you feel undervalued and under-resourced, like you are not good enough for your job. You may begin to blame others for not having the resources or processes that will help you overcome the obstacles of getting your work done. You might start to shame yourself and beat yourself up for not being able to handle things.
- This is in contrast to how you felt in the zealot phase or when you started the job. Maybe you did feel under-appreciated or undervalued at an earlier point, but you said to yourself, “its okay, these families need me".
- You become impatient, irritable, moody, angry.
Withdrawal Phase
- In the withdrawal phase you are tired all the time. Your sleep patterns are inconsistent. You may sleep all the time or not sleep enough. You may experience difficulties getting to sleep, or you wake up in the middle of the night and you can’t fall back to sleep.
- You may experience deficits in your immune system, getting colds constantly that never seem to clear up.
- You might start to experience the trap of self-entitlement, meaning you begin justifying your negative and maladaptive behaviours because of the positive things you stand for and the positive nature of your work. “I worked overtime this week so it’s okay if I get wasted this weekend, I deserve it.”
- You may experience difficulty concentrating, confusion, spaciness, racing and blurring thoughts. Your work starts to blend in with each other, making it hard to distinguish between the families you are working with.
- You may start to withdraw, neglect, and detach yourself from your clients, friends, family, and co-workers.
- The negative consequences of this phase include using negative coping mechanisms like substance use (smoking, alcohol, and other substances that are used and misused).
- There is a potential for thoughts of self-harm or harming others arises.
Zombie phase
- You begin feeling like you are on autopilot. You feel less confident in your work and notice you are making mistakes.
- You not only feel disconnected from yourself and others, but from your role in your profession. You begin to doubt your abilities, and your confidence that you are doing good work begins to disappear.
- You may feel like you have nothing left to give, whether that is to the people you are working with, your friends and family, and yourself.
- You feel depleted, empty, and numb.
- Again, there are the potential negative consequence described in the withdrawal phase such as substance use, negative coping mechanisms, and self-harm.
Self Care
- Minimize trauma input outside of work (TV, news, etc.)
- Meditation, mindfulness, exercise, yoga
- Find time for yourself every day
- Check-in with your emotions. Sit quietly and just name without judgment what you’re feeling.
- Delegate tasks at work and at home. Try not to take your work home with you (literally and figuratively)
- Have a transition from work to home (changing clothes, short walk)
- Take another route to work. Mixing up your routine in small ways creates new neural pathways in the brain to keep it healthy.
- Declutter and redecorate your workspace
- Unplug for an hour. Switch everything to airplane mode and free yourself from the constant bings of social media and email.
- Join a supervision/peer support group
- Be selfish. Do one thing today just because it makes you happy.
- Attend workshops/professional training
- Ask for help—big or small, but reach out.
- Scratch off a lurker on your to-do list, something that’s been there for ages and you’ll never do.
- Start a compliments file. Document the great things people say about you to read later.
- Reflect on three good things that happen every day
- Cut yourself a break
- Say no to strenuous demands more, and yes to more self-care
References
Figley, C. R., & Roop, R. G. Compassion fatigue in the animal-care community. Humane Society Press, 2006. https://animalstudiesrepository.org/cgi/viewcontent.cgi?article=1004&context=ebooks
Lee, E., Esaki, N., Kim, J., Kirkland, K., & Mitchell-Herzfeld, S. (2013). Organizational climate and burnout among home visitors: Testing mediating effects of empowerment. Children and Youth Services Review, 35, 594-602.
Lombardo, B., Eyre, C., (Jan 31, 2011) "Compassion Fatigue: A Nurse’s Primer" OJIN: The Online Journal of Issues in Nursing Vol. 16, No. 1, Manuscript 3. doi: 10.3912/OJIN.Vol16No01Man03
Miller, B. & Sprang, G. (2017). A components-based practice and supervision model for reducing compassion fatigue by affecting clinician experience. Traumatology, 23(2), 153-164. doi: http://dx.doi.org/10.1037/trm0000058
Newell, J. M. & MacNeil, G. A. (2010). Professional burnout, vicarious trauma, secondary traumatic stress, and compassion fatigue: A review of theoretical terms, risk factors, and preventive methods for clinicians and researchers. Best Practices in Mental Health, 6(2), 57-68
Raab, K. (2014). "Mindfulness, self-compassion, and empathy among health care professionals: a review of the literature." Journal of health care chaplaincy, 20(3), 95-108. www.h-partners-for-life.com/wp-content/uploads/2017/04/Mindfulness-Self-Compassion-and-Empathy-Among-Health-Care-Professionals-A-Review-of-the-Literature.pdf
Open configuration options
Resources
Crisis Prevention Institute https://www.crisisprevention.com/Blog/August-2015/Compassion-Fatigue
Compassion Fatigue Awareness Project http://www.compassionfatigue.org/pages/resources.html
Life Stress Test http://www.compassionfatigue.org/pages/lifestress.html
Empathy Test http://www.tarameyerrobson.com/empath-test/
Compassion Fatigue Self Test https://www.crisisprevention.com/Blog/August-2015/Compassion-Fatigue
Professional Quality of Life Measure https://proqol.org/
Figley Institute http://www.figleyinstitute.com/indexMain.html
Self-Care Resource Center - https://www.apa.org/helpcenter/self-care